In 2011, Judy Huie-Kennedy was diagnosed with stage 3B cervical cancer, and the journey to a cancer-free status in the following years was arduous, including two rounds of intense chemotherapy, radiation treatment and a hysterectomy.
Getting screened and diagnosed was “half the battle,” Huie-Kennedy told the Bronx Times.
The other half of that battle, for many, is insurance or lack thereof.
Cervical cancer is one of the most common forms of gynecologic cancers, with 6 in 1,000 women receiving a cervical cancer diagnosis at some point in their lifetime. But uninsured individuals and people with Medicaid are the most likely populations to be underscreened for cervical cancer, according to a study published by JAMA Network.
Montefiore Einstein Cancer Center’s annual See, Test & Treat event — held on May 20 at the Greene Medical Arts Pavilion in Williamsbridge — is aimed at getting women ages 21-64 free breast cancer and cervical cancer screenings.
“To me, it’s very important because some of the reasons why people don’t go to see their doctors, their providers, is that they may be afraid or feel it’s necessary,” said Huie-Kennedy, a longtime market specialist at Montefiore Medical Center. “But the bigger thing is they don’t have insurance and if they don’t have insurance, they can’t afford to pay, and they just let it go.”
Huie-Kennedy’s become a major part of Montefiore’s See, Test & Treat event, which started offering screenings in 2013. Taking on the role as the program’s project manager since 2018, Huie-Kennedy is motivated by her own cancer diagnosis and desire to bridge healthy equity gaps for Bronx women.
“I think by 2018 (See, Test & Treat) became more of a mission for me. It meant more just to see these women who were so fearful of getting the diagnosis, and we always had somebody there who was from either one of the cervical cancer societies or one of the oncologist providers that volunteered to speak with them to try and calm them down,” she said. “I truly believe that having the diagnosis is half the battle.”
According to the city’s health department, each year about 110 women die from cervical cancer and 430 women are newly diagnosed.
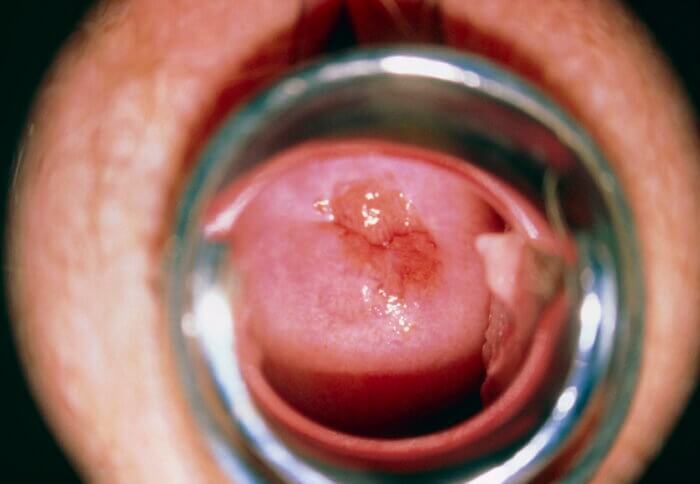
Data analysis of four decades of Bronx rates of cervical cancer show that while mortality rates from the cancer steadied around 20 deaths per year, the diagnoses rates fell from 80 diagnoses to 60 in 2020.
But some of those declining detection rates could be due to lack of screenings, health officials told the Bronx Times.
Regular cervical cancer screenings, such as Pap tests, can help identify and treat precancerous lesions or cancers, and individuals who receive diagnoses of early-stage cervical cancer have a five-year survival rate of more than 90%.
But when it comes to access to health care in the U.S., the focus is often on health insurance — whether people have it, and what it covers.
Findings from a recent Kaiser Family Foundation study cite 44% of uninsured women in the U.S. ages 50-64, who have not had a mammogram in the past two years say this is because they could not afford one.
“Women with higher incomes and those with higher educational attainment are more likely than women with lower incomes and less educational attainment to know that annual check-ups for women and cervical cancer screenings must be covered without cost sharing,” according to the study.
Bronx residents Iriesha Thomas, 36 and Chernice Boyd, 31, told the Bronx Times they haven’t received a Pap test since the early stages of the COVID-19 pandemic, and changes in employment factored in the decision to bypass regular screenings.
“As a Black woman, you just don’t feel seen or heard in many doctor’s offices,” said Boyd. “But when you lose a job that gives you health benefits … covers screenings and stuff like that, and you lose it, it gets to be overwhelming to manage your health when it’s expensive.”
Limited health literacy, a Harris poll conducted by Becton, Dickinson and Company found, also posed a barrier to cervical cancer screening.
More than 8 in 10 women said they didn’t know how often they should get a Pap test, and 51% said they were unaware of how often they should get an HPV tested.
Researchers found that in areas of the U.S. that passed mandates on paid sick leave, cancer screening rates inched up in the years afterward. Breast cancer screening rose by roughly 3%, while colon cancer screening increased by 6-8%.
And being uninsured or receiving health insurance through Medicaid accounted for more than half of racial inequities in advanced-stage cervical cancer diagnoses, JAMA Network researchers also found.
Black and Hispanic or Latina women are more likely than white women to receive a diagnosis of and to die of cervical cancer. An individual’s health insurance status, researchers suggested, is one of the modifiable risk factors that could reduce these persistent cervical cancer mortality inequities among Black populations.
According to MedicalNewsToday, Black women are 80% more likely to die from cervical cancer than white women. The overall five-year survival rate for Black women is around 56%, lower than the compared rate of 68% for white women.