On one of our first days of medical school at Columbia University, a physician who works in a private family medicine practice after starting out in a community hospital in Washington Heights came to speak with us about the practice of family and internal medicine in New York City. When asked why they had made this transition, they spoke about experiencing burnout from the worse outcomes associated with lower socioeconomic status, such that they switched to private practice for patients without those barriers. Our knee-jerk response was to fault the individual physician for giving up in the face of the systemic obstacles that health care providers across the nation face on a daily basis. Upon further reflection, however, what we found unsettling was not the physician’s choice, but the existence of barriers so pervasive that they were not only causing rampant provider burnout, but also leading to catastrophic patient outcomes and health inequities.
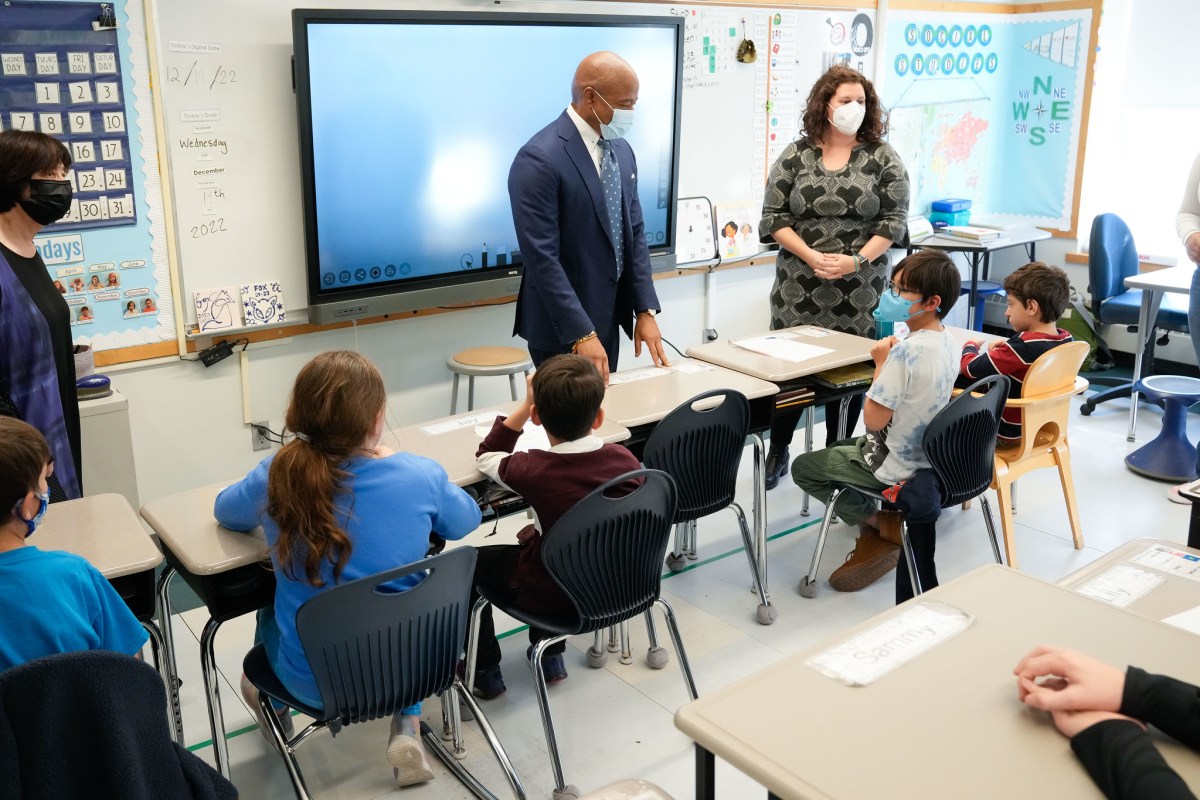
The obstacles facing doctors working in public hospitals and clinics are obvious. The Washington Heights, Hamilton Heights, Inwood and Harlem communities surrounding New York-Presbyterian Hospital (NYP) experience glaring systemic health disparities. You see it in the higher rates of diabetes, hypertension, HIV and teen pregnancy experienced here compared with the rest of Manhattan. The source of these health disparities is equally clear: Washington Heights adults are almost twice as likely to be without health insurance and in need of medical care than the rest of Manhattan (NYC.gov). For members of these communities, slower, less adequate and less well-resourced care as a result of inadequate insurance and socioeconomic status is not the exception but the rule (Tikkanen, 2017). Of course, this isn’t just a Columbia-NYP problem. It’s a dichotomy that exists in every major American city. It transcends individual institutions and is a symptom of the deep inequities built into our health care system.
Although we are newcomers to the field, we hear the voices of the physicians who came before us and feel the urgency to advocate for change — before we face the burnout that the current system inflicts on so many healthcare workers today. Our perspectives have led us to the inescapable conclusion that we must immediately and comprehensively reorganize healthcare into a unified system that upholds access, equity, and quality in health. This system must be rooted in a simple principle: that everyone deserves a right to healthcare. With the New York Health Act (NYHA), New York has an unique opportunity to make this a reality.
NYHA is a visionary piece of legislation that would establish a single-payer health plan and provide universal coverage to all New York residents. The bill, which has sponsorship in both houses of the state Legislature, would cover every New Yorker under a centrally negotiated and comprehensive plan, regardless of income, employment and immigration status. The NYHA plan would cover traditional inpatient and outpatient medical care, along with benefits like rehabilitation, dental, hearing and vision care. All health care providers would accept the insurance plan, eliminating the convoluted navigation of in- and out-of-network care.
The NYHA would reduce the financial toxicity of our current system, in which even having insurance does not guarantee access to care and costs are often hidden until the hospital bill arrives. Despite the fact that 9 in 10 Americans have some form of health insurance, there are estimates showing that up to 62.1% of bankruptcies in America are due to medical bills (Amadeo, 2021). The NYHA plan would improve upon current insurance by eliminating deductibles, copays and higher out-of-network costs, decreasing health care costs for 90% of patients in New York. (Rodberg, 2019).
The funding would come from a progressive payroll tax — 80% of which would be paid by employers — and capital gains taxes. That, plus the consolidation of existing state and federal funds for Medicare, Medicaid, Family Health and Child Health Plus, would pay for the $139 billion legislation. This centralized system would also reduce administrative costs, which currently account for 15-25% of total health care expenditures, by an estimated $20.2 billion. The net savings from this plan are estimated at $11.3 billion, even as more New Yorkers gain coverage and enjoy more benefits, and Medicare and Medicaid enjoy higher reimbursement rates.
The embattled history of health reform in our country has seen many proposals and changes over the years, and the Affordable Care Act of 2010 was an important step in the right direction. Unfortunately, when it comes to health equity, expanding the ACA alone is not enough, as it ultimately preserves the fundamental disparities built into our existing system. Even if public insurance plans are offered to compete alongside private ones (commonly called a “public option”), it inevitably perpetuates the current, tiered system that separates patients based on their insurance status. Individuals with private insurance plans will disproportionately receive first-rate services at distinguished institutions like NYP. Meanwhile, those who can only afford cheaper plans will be confined to certain networks, providers and resources, and will continue to suffer from poorer health outcomes. This is precisely why the NYHA is the necessary first step we need toward health care that is not only accessible and efficient, but also equitable.
As medical students, we are among the countless people in this country that interface everyday with the injustice perpetuated by an inadequate health care system that prioritizes profit over equitable care. As we learned all too soon, these barriers harm both patients and providers. The NYHA gives us a chance to start again with a clean slate and build a single-payer health system that delivers the promises of modern medicine to all. We will not tolerate the systematic discrimination against the lives and wellbeing of New Yorkers rampant in our current system, and we are confident that the New York Health Act can drastically change health care for the better. We call on the New York State Legislature and Gov. Kathy Hochul to pass NYHA in 2022.
Anna Koerner, Karl Reis, Kevin Wang, Dean Strup, Hsin Yi Chen, Hannah Weinstein and Emma Tucker are medical students at Columbia University and members of the Columbia University chapter of Students for a National Health Program (SNaHP), which is the student-arm of Physicians for a National Health Program (PNHP).